What is COPD and Why Treatment Matters
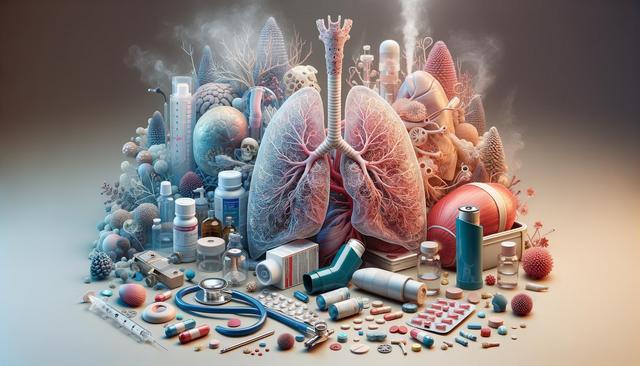
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease that includes conditions such as emphysema and chronic bronchitis. It causes airflow blockage and breathing-related problems, which can worsen over time if not properly managed. Treatment is essential not only to alleviate symptoms but also to slow progression, reduce complications, and improve overall quality of life. Understanding the nature of COPD helps individuals and caregivers make informed decisions about care and lifestyle adjustments.
Symptoms of COPD can include chronic cough, shortness of breath, and frequent respiratory infections. Because the disease can affect people differently, treatment plans are typically customized to address specific conditions and severity levels. Early diagnosis and consistent management can greatly influence the effectiveness of treatment strategies.
Medication Options for COPD Management
Medications play a central role in treating COPD. They help open airways, reduce inflammation, and prevent exacerbations. Depending on the stage of the disease, healthcare providers may recommend different types of medications, including:
- Bronchodilators: These relax the muscles around the airways, making breathing easier.
- Inhaled corticosteroids: These reduce airway inflammation and help prevent flare-ups.
- Combination inhalers: These include both bronchodilators and steroids for better symptom control.
- Phosphodiesterase-4 inhibitors: Used for severe COPD with chronic bronchitis to reduce inflammation and relax airways.
- Antibiotics: Prescribed to treat or prevent infections that can worsen COPD.
It’s important for patients to use medications as prescribed and report any side effects or changes in symptoms to their healthcare provider. Regular follow-ups and lung function tests may be needed to adjust treatment plans effectively.
Pulmonary Rehabilitation and Lifestyle Adjustments
Pulmonary rehabilitation is a structured program that combines education, exercise training, nutritional advice, and counseling. It’s designed to help patients live more actively and manage their condition better. Participants often report improved breathing, increased stamina, and a better understanding of their disease. Key components of a pulmonary rehabilitation program include:
- Supervised exercise sessions to strengthen respiratory muscles
- Breathing techniques such as pursed-lip breathing
- Advice on healthy eating and maintaining a balanced diet
- Support for quitting smoking, which is crucial for slowing disease progression
In addition to rehabilitation, patients are encouraged to make lifestyle changes such as avoiding air pollutants, staying physically active within limits, and getting vaccinated against flu and pneumonia to prevent infections.
Oxygen Therapy and Surgical Interventions
For individuals with advanced COPD, oxygen therapy may be necessary. This involves using a device to deliver extra oxygen to the lungs, helping to relieve breathlessness and improve energy levels. Oxygen therapy can be administered in various ways, including concentrated oxygen tanks or portable concentrators, depending on the patient’s mobility and lifestyle needs.
In some cases, surgical treatments may be considered. These options are typically reserved for those who do not respond well to medications and rehabilitation. Surgical treatments may include:
- Bullectomy: Removal of large air spaces (bullae) that interfere with breathing
- Lung volume reduction surgery: Removing damaged lung tissue to allow healthier parts to function more effectively
- Lung transplant: Considered for younger patients with very severe COPD and no other treatment options
Each of these interventions carries risks and benefits, and they are carefully evaluated by medical teams to ensure suitability for the individual.
Monitoring and Long-Term Management Strategies
Managing COPD is an ongoing process that requires regular medical attention and self-care. Patients are advised to monitor their symptoms closely and recognize early signs of exacerbations, such as increased coughing, changes in mucus color, or more difficulty breathing. Early intervention can often prevent hospitalizations and further lung damage.
Long-term management involves:
- Routine check-ups with healthcare providers
- Use of spirometry tests to track lung function
- Adjusting medications as needed
- Staying current with vaccinations
- Maintaining a healthy lifestyle with a focus on diet, exercise, and avoiding triggers
Support groups and counseling can also be valuable for emotional well-being, as living with a chronic illness can be challenging. Family members and caregivers play an important role by offering support and helping with treatment adherence.
Conclusion: Taking Control of COPD Through Comprehensive Care
Living with COPD involves more than just treating symptoms—it’s about adopting a comprehensive care approach that includes medication, rehabilitation, lifestyle changes, and regular monitoring. While COPD is a chronic condition, many individuals find that with the right support and medical guidance, they can lead active and fulfilling lives. Staying informed, working closely with healthcare providers, and making health-conscious choices are essential steps for anyone managing COPD.



Leave a Reply