What Is a Blood Clot and Why Does It Matter?
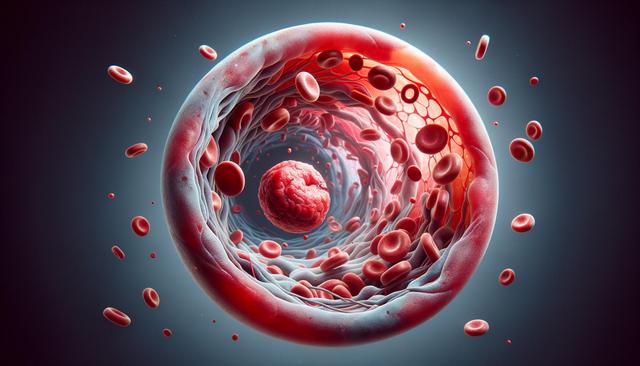
A blood clot is a clump of blood that has changed from a liquid to a gel-like or semisolid state. While clotting is a necessary mechanism to stop bleeding after an injury, clots that form inappropriately within blood vessels can cause severe health issues. These clots can restrict or block blood flow, potentially leading to complications such as deep vein thrombosis (DVT), pulmonary embolism (PE), heart attack, or stroke. Understanding how and why blood clots form is essential to managing the risk, especially for individuals with underlying health conditions, a sedentary lifestyle, or a family history of clotting disorders.
Blood clots can be classified based on their location and nature. The two primary types are:
- Arterial clots – usually associated with atherosclerosis and can lead to heart attacks or strokes.
- Venous clots – often occur in the deep veins of the legs and can travel to the lungs causing a pulmonary embolism.
Recognizing the signs of a clot, such as swelling, pain, redness, or shortness of breath, is crucial for early intervention and preventing complications.
Common Risk Factors and Contributing Conditions
Several factors can increase the likelihood of developing blood clots. These range from genetic predispositions to lifestyle-related elements. Knowing these risk factors can help individuals and healthcare providers make informed decisions about prevention and monitoring.
Key risk factors include:
- Prolonged immobility, such as during long flights or bed rest
- Recent surgery or trauma, especially to the lower limbs
- Obesity and sedentary lifestyle
- Smoking and excessive alcohol consumption
- Use of hormone replacement therapy or birth control pills
- Pregnancy and the postpartum period
- Certain chronic illnesses like cancer, diabetes, or autoimmune disorders
In addition, inherited conditions like Factor V Leiden or prothrombin gene mutation increase the risk of abnormal clotting. A comprehensive review of an individual’s health history is essential to identify and address these contributing factors.
Diagnosis and Initial Treatment Options
Timely diagnosis of a blood clot is crucial in preventing serious complications. Healthcare professionals typically use a combination of physical exams, medical history, and diagnostic imaging techniques such as ultrasound, CT scans, or MRI to confirm the presence of a clot. Blood tests like the D-dimer test can also help detect abnormal clotting activity.
Once diagnosed, initial treatment aims to prevent the clot from growing and reduce the risk of further clot formation. Commonly used treatments include:
- Anticoagulant medications – such as heparin or warfarin, which thin the blood
- Thrombolytic therapy – in severe cases, drugs may be used to dissolve clots more quickly
- Supportive measures – compression stockings and hydration to improve circulation
The choice of treatment depends on the type, size, and location of the clot, as well as the patient’s overall health. Treatment plans should be customized and closely monitored by healthcare professionals to ensure safety and effectiveness.
Long-Term Management and Lifestyle Adjustments
Managing blood clots doesn’t stop after initial treatment. Long-term care is critical to prevent recurrence and improve quality of life. Patients who have experienced a clot often require ongoing anticoagulation therapy, sometimes for life, depending on their risk profile.
Key elements of successful long-term management include:
- Regular follow-up appointments and blood tests to monitor medication effects
- Maintaining a healthy weight and active lifestyle
- Avoiding prolonged periods of inactivity, especially during travel
- Staying hydrated and wearing compression garments if advised
- Discussing all medications and supplements with a healthcare provider to avoid interactions
Dietary considerations also play a role, particularly for those on anticoagulants that can be affected by vitamin K intake. A registered dietitian or healthcare provider can offer personalized guidance on nutrition and activity plans to support vascular health.
Preventing Future Blood Clots
Prevention is a key strategy in managing blood clot risks, especially for individuals with a history of clotting issues or those exposed to known risk factors. While not all clots can be prevented, certain measures can significantly reduce the likelihood of occurrence.
Preventive strategies include:
- Routine health screenings and early detection of underlying conditions
- Use of prophylactic anticoagulants before and after surgery when appropriate
- Staying active, especially during long periods of sitting or bed rest
- Educating patients and caregivers on the signs and symptoms of blood clots
Employers and healthcare facilities can also play a role by encouraging regular movement and providing ergonomic setups that promote circulation. Raising awareness about blood clot prevention can lead to better health outcomes and fewer emergency situations.
Conclusion: Managing Blood Clots with Awareness and Action
Understanding blood clot treatments and risk management is essential for those affected and for individuals at increased risk. While blood clots can be serious, they are often manageable with timely intervention, structured treatment plans, and lifestyle adjustments. By staying informed and proactive, patients can work with healthcare providers to minimize risks and lead healthier lives. Education, regular monitoring, and preventive care are foundational steps in reducing the impact of blood clots and maintaining long-term vascular health.



Leave a Reply