What Is a Blood Clot and Why It Matters
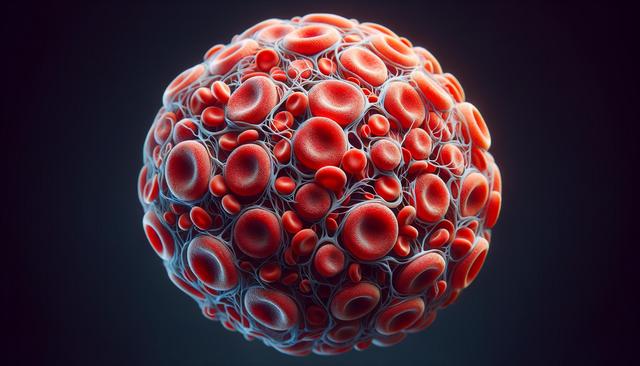
A blood clot, or thrombus, is a gel-like mass formed by platelets and fibrin in the blood to stop bleeding. While clotting is a natural and necessary function, clots that develop inappropriately within blood vessels can pose serious health risks. These clots can obstruct blood flow, potentially leading to conditions such as deep vein thrombosis (DVT), pulmonary embolism (PE), or stroke. Understanding how and why blood clots form is the first step in managing their impact. Clots can develop from a variety of causes, including prolonged immobility, surgery, inherited clotting disorders, or certain chronic conditions such as cancer or autoimmune diseases.
Blood clots may either be arterial or venous. Arterial clots often result in immediate symptoms such as pain, paralysis, or organ damage. Venous clots, such as those found in DVT, can progress more slowly but may still lead to life-threatening outcomes if they travel to the lungs. Recognizing symptoms early—such as swelling, redness, or pain in the limbs—can be crucial in seeking timely treatment. Prevention and awareness are key, especially for individuals at higher risk due to lifestyle or medical history.
Diagnosing Blood Clots: Methods and Importance
Timely diagnosis of a blood clot is critical to prevent complications. Healthcare providers use a range of diagnostic tools to detect and assess clots. The choice of test often depends on the suspected location and severity of the clot. Common diagnostic methods include:
- Ultrasound imaging – primarily used for detecting DVT in the legs.
- D-dimer blood test – measures clot degradation products in the blood.
- CT or MRI scans – helpful in identifying clots in the lungs, brain, or abdomen.
- Venography – an X-ray test using contrast dye to visualize veins.
Each method has its strengths and limitations. For example, while a D-dimer test is useful for ruling out a clot in low-risk individuals, it cannot confirm the presence of a clot alone. Imaging tests provide a more definitive diagnosis but may not be immediately available in all settings. For individuals with recurring symptoms or a history of clotting disorders, regular monitoring may be recommended. Diagnosing blood clots early not only saves lives but also helps tailor personalized treatment strategies for better outcomes.
Treatment Options for Blood Clots
Treating a blood clot involves stopping its growth, preventing new clots from forming, and minimizing the risk of complications. The specific treatment depends on the type, size, and location of the clot, as well as the patient’s overall health. Common treatment approaches include:
- Anticoagulants – also known as blood thinners, these medications prevent further clotting but do not dissolve existing clots.
- Thrombolytics – used in emergency situations to dissolve large, life-threatening clots.
- Compression stockings – help manage symptoms and prevent clot recurrence in the legs.
- Surgical intervention – rarely, a clot may need to be removed physically in severe cases.
Each treatment comes with its own set of risks and benefits. For example, anticoagulants require careful monitoring to avoid bleeding complications, while thrombolytics are typically reserved for acute events due to their potency. Long-term treatment may also be necessary for individuals with persistent risk factors. Collaboration between patients and healthcare providers is essential in developing a management plan that aligns with both medical needs and lifestyle considerations.
Preventing Blood Clots Through Lifestyle and Medical Strategies
Prevention plays a vital role in reducing the risk of blood clots, particularly for high-risk individuals. Lifestyle adjustments and medical interventions can significantly decrease the likelihood of clot formation. Key preventive measures include:
- Staying physically active – regular movement improves circulation and reduces venous stasis.
- Maintaining a healthy weight – obesity is a known risk factor for clot development.
- Staying hydrated – adequate fluid intake supports healthy blood viscosity.
- Wearing compression garments – especially useful during long periods of immobility like travel or hospitalization.
- Following medication protocols – individuals on anticoagulants should adhere strictly to dosing schedules.
Healthcare providers may also recommend routine screenings for individuals with a genetic predisposition to clotting or those undergoing surgical procedures. Education about symptoms and when to seek help is equally important. Empowering patients with knowledge and practical tools can lead to better prevention and early intervention. By integrating these strategies into daily routines, many individuals can substantially reduce their risk of experiencing a serious clot-related event.
Long-Term Management and Monitoring
For individuals who have experienced a blood clot, long-term management is critical to prevent recurrence and maintain quality of life. Ongoing care often includes regular check-ups, blood tests, and adjustments to medication. Factors influencing long-term management include the cause of the initial clot, underlying conditions, and how well the patient tolerates treatment. Some individuals may require lifelong anticoagulation therapy, particularly if the clot occurred without an identifiable trigger or was associated with a chronic condition.
Patients are encouraged to be proactive in their care by:
- Monitoring for signs of new clots or bleeding complications.
- Maintaining open communication with healthcare providers about any side effects or concerns.
- Making informed decisions about activity levels, travel, and diet—especially regarding foods that interact with medications.
- Staying current with follow-up appointments and lab work.
Support groups and educational resources can also provide valuable assistance for those navigating long-term treatment. Understanding that blood clot management is not a one-time event but a continuous process helps individuals take control of their health more effectively. With careful attention and the right support, the risks associated with blood clots can be significantly minimized.
Conclusion: Promoting Awareness and Proactive Health
Blood clots can pose serious health risks, but with proper awareness, timely intervention, and consistent care, complications can often be prevented or effectively managed. Whether you are at risk, have experienced a clot, or are supporting someone who has, understanding the range of treatment and prevention strategies is essential. By working closely with healthcare professionals and adopting a proactive approach, individuals can navigate the challenges of blood clot management with greater confidence and control. Staying informed and engaged remains one of the most effective ways to maintain long-term vascular health.



Leave a Reply